PATHOPHYSIOLOGY Multiple Choice Questions :-
1. Leptomeningitis is an inflammatory process that is localized to the interfacing surfaces of the _______ and the _________, where ______ flows?
A. Dura, Pia, CSF
B. Arachnoid, Pia, Blood
C. Pia, Arachnoid, CSF
D. Dura, Arachnoid, CSF
Answer: C
2. Which of the following is TRUE about Pachymeningitis?
A. Inflammation of the Pia
B. Usually a consequence of traumatic brain injury.
C. The arachnoid acts as a barrier to infection.
D. The inflammation is restricted to the outer surface of the brain.
Answer: B
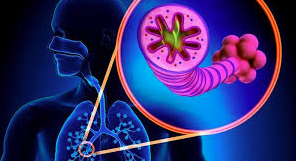
3. In the earliest stages of pulmonary edema all of the following are true except:
A. Fluid tracks through the interstitium of the thin side of the blood Gas barrier to the perivascular and peribronchial spaces.
B. There is no increase in lung lymph flow.
C. Fluid floods the alveoli one by one.
D. The hydrostatic pressure in the interstitium probably falls.
E. Cuffs of fluid collect around the small arteries and veins.
Answer: E
4. Which of the following is not true of Bacterial Meningitis organisms and age?
A. E. Coli and Group B strep are most commonly found in neonates with bacterial meningitis
B. Group A strep and H. Pylori are most commonly found in adolescents with bacterial meningitis.
C. H. influenza is usually fuond in infants 3 months-3 years old with bacterial meningitis.
D. Strep pneumococcus is usually found in adults with bacterial meningitis.
E. N. meningitidis is usually found in military barracks when bacterial meningitis is going around.
Answer: B
5. What is the most difinitive diagnostic index of meningitis?
A. PMN’s in the CSF
B. PMN’s in the blood
C. RBC’s in the CSF
D. Purulent discharge in the ears
E. Elevated white count
Answer: A
6. ________ are the hallmark of meningitis caused by tuberculosis, viral meningitides, and chronic fungal infections (cryptococcal meningitis.)
A. Macrophages
B. Lymphocytes
C. Eosinohpils
D. Monocytes
Answer: B
7. Grossly, the brain discloses an exudate of PMN’s and fibrin which opacifies the _________, and giving a _ ___or _________ white appearance, usually over the convexities as well as the base of the brain.
A. pia, creamy or white
B. arachnoid, yellow or purulent
C. Arachnoid, creamy or white
D. Dura, Yellow or purulent
E. Arachnoid, grey or cloudy
Answer: C
8. influenza elicits a dense leukocytic exudate, which is rich in fibrin over the convexities and therefore creates a barrier to antibiotics.
A. True
B. False
Answer: A
9. Because the pia is so delicate, it is an ineffective barrier against the spread of infection and typically does not prevent spread to the underlying brain.
A. True
B. False
Answer: B
10. Which of the following is not a clinical manifestation of Bacterial Meningitis?
A. Head ache
B. Convulsions in adults
C. fever
D. If untreated, coma and death
E. Vomiting
Answer: B
11. The classic signs of meningeal infection include all of the following EXCEPT:
A. Cervical rigidity
B. Kernig sign
C. Head retraction
D. Murphy’s sign
E. Brudzinski sign
Answer: D
12. Which diseased is defined as a neurologic disorder characterized pathologically by the loss of neurons in the Substantia Nigra and clinically by tremors at rest, muscular rigidity, expressionless face, and emotional lability.
A. Bacterial Meningitis
B. Alzheimers Disease
C. Viral Meningitis
D. Multiple Sclerosis
E. Parkinsons Disease
Answer: E
13. Which of the following is NOT true of Parkinson’s disease?
A. Most commonly occurs in white males
B. Typically effects those in the 6th-8th decade of their life.
C. Genetic factors do not play a role (except for a rare autosomal dominant disorder)
D. The vast majority of cases are idiopathic.
E. The disease has been recorded after viral encephalitis and after the intake of a toxic chemical (MPTP. .
Answer: A
14. It has been suggested that Parkinsons disease is an acceleration of normal age related changes.The changes being referred to primarily have to do with the ___________ which relays information to the _______ through _________ synapses.
A. Brain stem, sympathetic chain, adrenergic
B. Cerebral cortex, cranial nerves, muscarinic
C. Substantia Nigra, basal ganglia, dopaminergic
D. Prefrontal cortex, afferent neurons, cholinergic
E. Medulla oblongota, efferent neurons, achetylcholinestergic
Answer: C
15. What type of infection resulting in injury (gross loss of pigmentation) to the substantia nigra occured during the infuenza pandemic of 1916-1920 which lead to the clinical expression of “postencephalitic parkinsonism.”
A. Bacterial meningitis
B. Acute hepatitis
C. Cholelithiasis
D. Sinusitis
E. von Economo Encephalitis
Ans: E
16. Microscopically, what are the changes seen in Parkinson’s disease?
A. Loss of pigmentation in the substantia nigra
B. Residual atrophic nerve cells are seen known as “Hewey Bodies”
C. Pigmented neurons are scarce with small extracellular deposits of melanin, from necrotic neurons.
D. Loss of pigmentation in the Locus Ceruleus
Answer: C
17. Asterixis is liver flap.
A. Yes
B. No
Answer: A
18. Blood from GI tract enters the liver thru ________?
A. Hepatic vein
B. Hepatic artery
C. Portal artery
D. Portal vein
Answer: D
19. All of the following are clinical manifestations of Parkinson’s disease EXCEPT:
A. Depression
B. Hypertonia
C. Hypotonia
D. Dimentia
E. Akinesia
Answer: C
20. True or false: In early parkinsonism, Levadopa is beneficial, however this therapy does not rectify the underlying disorder, and several years later, becomes ineffective.
A. True
B. False
Answer: A
21. Other causes of Parkinson-like symptoms include all of the following EXCEPT:
A. Spider bites (black widow, tunnel spider)
C. Poison (Carbon monoxide, Manganese)
D. Hydrocephalus
E. Tumors (Near the basal ganglia)
Answer: A
22. This disease is known as an insidious and progressive neurologic disorder characterized by a loss of memory, cognitive impairment, and eventual dementia?
A. Parkinson’s disease
B. Age-related psychosis
C. Alzheimers Disease
D. Multiple Sclerosis
E. Acute Hemorrhagic Meningitis
Answer: C
23. True or False: Alzheimers Disease is restricted to patients younger than 65 years of age and already diagnosed with presenile dimentia.
A. True
B. False
Answer: B
24. Which of the following is a feature of Alzheimers Disease?
A. Advances of our pathologic understanding of AD relate to alpha-protein amyloid deposition in senile plaques.
B. Plaques located in the spinal cord are linked to intelectual funciton and are a constant feature of AD
C. Beta protein amyloid is found in the walls of the cerebral vessels may be the origin of deposits found in the brain in AD.
D. The pathogenisis of AD is fully understood
E. World wide, AD is the least common cause of dementia in the elderly, accounting for less than half of all the cases.
Answer: C
25. Current advances in AD include the understanding of Neurofilbrillary tangles, which are paired _______ filaments. These filaments, consist of an abnormal form of a normally occuring ___________ protein. When normal, the protein is responsible for proper _________ transport.
A. Pleated, macrotubule-associated, lipid
B. Helical, microtubule-associated, axonal
C. Round, cytoskeletal-associated, active
D. Helical, macrotubule-associated, lipid
Answer: B
26. Which of the following is NOT true of the gross Alzheimers brain?
A. Loss of neurons and neuritic processes
B. Narrow gyri
C. Widened sulci
D. Unilateral cortical atrophy
E. Atrophy in frontal, parietal, temporal, and hippocampal cortices.
Answer: D
27. True or False: The Alzheimers brain loses roughly 200 gms in an interval of 3-8 years.
A. True
B. False
Answer: A
28. What are discrete spherical masses of sliver-staining neuritic processes surrounding a central amyloid core?
A. Lewy Bodies
B. Neurofibrillary tangles
C. Signet ring cells
D. Hewey Bodies
E. Senile (neuritic) plaques
Ans: E
32. The combination of clincal assessment and modern radiologic methods allow for acurate diagnosis in 80-90% of cases however, which of the following is necessary for a difinitive diagnosis.
A. Biopsy
B. Endoscopy
C. Pathologic examination of vessels in the brain
D. Pathologic examination of brain tissue
Answer: D
33. An 85 year old female patient gradual loss of memory, cognitive function, difficulty with language, and changes in behavior. What is the most likely diagnosis?
A. Multiple Sclerosis
B. Alzheimers Disease
C. Parkinson’s Disease
D. Viral meningitis
Answer: B
34. True or False: Terminal bronchopneumonia is the usual cause of death in AD.
A. True
B. False
Answer: A
35. Which of the following is not true of Multiple Sclerosis?
A. A chronic demyelinating disease of the CNS
B. Characterized by numerous patches of demyelination througout the grey matter
C. It is the most common demyelinating disorder (prevelence 1 in 1000)
D. Disease effects both sensory and motor functions
E. Characterized by exacerbations and remissions over a period of years.
Answer: B
36. Risk factors for MS include all of the following EXCEPT:
A. Tropical climates
B. Most common in 40 year olds (uncommon before 14 and after 60 y.o).
C. Women afflicted twice as often as men
D. Possibly other infectious, genetic, and infectious etiology
Answer: A
37. Which of the following is true of genetic and immune factors related to MS?
A. A familial aggregation of the disease with an increased risk in 1st degree relatives.
B. Dizygotic twins show a 25% concordance for MS (2% for monozygotic)
C. Immune factors related to perivascular lymphocytes and macrophages with numerous CD4+, CD8+, and t-cells
D. Direct evidence exists for the involvement of certain viruses including mumps, rubella, herpes, and measles.
E. JC virus has recently been studied, due to its role in preventing demyelination in the CNS.
Answer: C
38. Which of the following is NOT true of the “hallmark of the disease” in MS?
A. The plaque is the hallmark of the disease
B. Usually situated in the white matter, but occassionaly breech the gray-white junction
C. Exhibit a preference for the optic nerves and chiasm and uniformly localizes in to the periventricular white matter.
D. Can also involve the cerebellum, brainstem, and spinal cord.
E. Usually 2-4 mm in size with a jagged, irregular contour
Ans: E
39. All of the following are true about MS, EXCEPT:
A. Histologically, there is a selective loss of myelin in a region of axonal preservation.
B. Perivascular inflammation lymophocytes and macrophages with focal edema.
C. Astrocytes traverse the aging plaque and the tissue becomes dense with glial processes.
D. As the plaque ages, it becomes less discrete and the edema progresses.
Answer: D
40. True or false: Some patients with MS exhibit a relentless course without any exacerbations or remissions.
A. True
B. False
Answer: A
42. Your 37 year old patient presents with blurred vision and vertigo. Due to a history of exacerbations and remissions you begin to suspect MS. Upon radiographic studies, where do you expect to find the initial lesion?
A. Optic nerves
B. Brain Stem
C. Prefrontal cortex
D. Spinal cord
E. Basal ganglia
Answer: B
43. You’re 37 year old patient presents with blurred vision and loss of vision altogether in one eye. Based on the patients age and her description of exacerbations and remissions, you begin to suspect:
A. Alzheimers Disease
B. Viral Meningitis
C. Bacterial Meningitis
D. Multiple Sclerosis
E. Myesthenia Gravis
Answer: D
44. Your 42 year old patient presents with weakness in both legs and numbness of lower extremities that bothers them intensely for 6-7 weeks and then subsides. This is the 3rd time they have been to your office because the symptoms keep coming back. You are beginning to suspect MS and expect to find what after radiologic testing?
A. A lesion at the optic nerve
B. A plaque in the brain stem
C. A plaque within the spinal cord
D. A lesion at the substantia nigra
E. A plaque within the basal ganglia
Answer: C
45. The degree of functional impairment with MS is variable, ranging from minor disability to severe incapacity. The range of symptoms include all of the following, EXCEPT:
A. Widespread paralysis
B. Severe nausea and vomiting
C. Dysarthria
D. Severe visual defects
E. Incontincence and dementia
Answer: B
46. True or false: In MS, patients usually die of respiratory paralysis or UTI’s in terminal coma 10-15 years after the onset of symptoms.
A. True
B. False
Answer: B
47. Acute/chronic inflammation cause by alcoholism, cholelithiasis, trauma, or cystic fibrosis, that presents with epigastric pain is called…
A. Renal failure
B. Hepatic failure
C. Diabetes Mellitus
D. Pancreatitis
Answer: D
48. Enzymes amylase and lipase are from the…
A. Liver
B. Pancreas
C. Lungs
D. Salivary glands
Answer: B
49. Right upper quadrant pain with nausea and vomiting, fever and a positive Murphy’s Sign is…
A. Cholelithiasis
B. Cholecystitis
C. Pancreatitis
D. Peritoneal abscess
Answer: B
50. What is not a function of calcium?
A. Bones and teeth
B. Blood coagulation
C. Cardiac and Nerve conduction
D. GI stimulation (peristalis.
E. Muscle contraction
Answer: D
PATHOPHYSIOLOGY Objective type Questions with Answers
51. What is not a factor needed for increasing or decreasing blood calcium?
A. Calcitonin
B. Vitamin D
C. Vitamin A
D. PTH
E. Kidneys
Answer: C
52. All are associated with hypocalcemia except…
A. Renal failure
B. Osteoporosis
C. Muscle cramps and tetany
D. Laryngospasm
E. Jaundice
Answer: E
54. Flank pain, dehydration, N/V, dysuria, and hematauria are all associated with what disease?
A. Cholelithiasis
B. Costochondritis
C. Nephrolithiasis
Answer: C
55. Big joints, pain in hands hips and feet, decrease of pain with rest are all associated with what?
A. Osteomyelitis
B. Osteoarthritis
C. Rheumatoid arthritis
D. Bone Cancer
Answer: B
56. Trichomonas is a result of a __________ infection.
A. Bacterial
B. Viral
C. Protozoal
D. Fungal
E. Parasitic
Answer: C
57. What is not a cause of testicular torsion?
A. Trauma
B. Genetics
C. Sports
D. Exercise
Answer: B
58. This disease loves the big toe, and patient may present with_______.
A. Gout, gallstones
B. Paranychia, appendicitis
C. Gout, kidney stones
D. Paranychia, kidney stones
Answer: C
59. D-dimer will be high or low in patients with blood clots?
A. High
B. Low
C. Neither
Answer: A
60. In the upright human lung, which of the following is greater at the apex than the base?
A. Blood flow.
B. Ventilation.
C. Alveolar PCO2.
D. Alveolar size.
E. Capillary blood volume.
Answer: D
61. Which of the following increases by the largest percentage at maximal exercise compared with rest?
A. PCO2 of mixed venous blood.
B. Alveolar ventilation.
C. Tidal volume.
D. Heart rate.
E. Cardiac output.
Answer: B
62. Which form of emphysema predominantly affects the apex of the lung?
A. That caused by ?1-antitrypsin deficiency.
B. Centriacinar emphysema.
C. Panacinar emphysema.
D. Paraseptal emphysema.
E. Unilateral emphysema.
Answer: B
63. A current hypothesis for the pathogenesis of emphysema is:
A. Damage to pulmonary capillaries by increased alveolar pressure.
B. Chronic stimulation of bronchial mucous glands by cigarette smoking.
C. Destruction of lung elastin by excessive action of neutrophil elastase.
D. Excessive amounts of exercise.
E. Hyperventilation at high altitude.
Answer: C
64. Alpha 1-antitrypsin deficiency:
A. Causes severe bronchitis with emphysema.
B. Results in emphysema at a relatively early age.
C. Is caused by infections in early childhood.
D. Is common in heterozygotes for the Z gene.
E. Tends to be most marked in the upper regions of the lung.
Answer: B
65. Patients with COPD with the type A presentation (as opposed to type B. tend to have:
A. More cough productive of sputum.
B. Smaller lung volumes.
C. Decreased lung elastic recoil.
D. More hypoxemia.
E. Greater tendency to develop cor pulmonale.
Answer: C
66. In a patient with severe bronchitis and emphysema, which of the following is likely to be normal?
A. FEV1.
B. FVC.
C. FEV1/FVC.
D. FEF25–75%.
E. None of the above.
Answer: E
77. The chief mechanism of hypoxemia in patients with COPD is:
A. Hypoventilation.
B. Diffusion impairment.
C. Ventilation–perfusion inequality.
D. Shunt.
E. Abnormal hemoglobin.
Answer: C
88. When a bronchodilator is administered to a patient during an asthma attack, which of the following typically decrease?
A. FEV1
B. FEV/FVC %
C. FVC
D. FEF25–75%
E. FRC
Ans: E
89. Concerning the use of ?-adrenergic agonists in asthma:
A. ?1-selective agonists are preferred to ?2 agonists.
B. They relax airway smooth muscle by decreasing the concentration of adenyl cyclase.
C. They reduce the concentration of intracellular cAMP.
D. They reduce airway inflammation.
E. They are usually given as tablets by mouth.
Answer: D
90. The type II alveolar epithelial cell:
A. Provides most of the structural SPport for the normal alveolar wall.
B. Cannot multiply.
C. Is formed when a type I epithelial cell divides.
D. Secretes surfactant.
E. Is metabolically inactive.
Answer: D
91. Histologic changes in diffuse interstitial pulmonary fibrosis typically include:
A. Infiltration of the alveolar wall with lymphocytes and plasma cells.
B. Breakdown of many alveolar walls.
C. Mucous gland hypertrophy in the bronchi.
D. Mucous plugging of airways.
E. Increased volume of the pulmonary capillary bed.
Answer: A
92. Features of diffuse interstitial pulmonary fibrosis include:
A. Cough productive of copious sputum.
B. Hemoptysis.
C. Rhonchi in both lungs.
D. Dyspnea especially on exercise.
E. Depressed diaphragms on the radiograph.
Answer: D
93. Pulmonary function tests in diffuse interstitial pulmonary fibrosis typically show:
A. Increased FEV1.
B. Increased FVC.
C. Increased FEV1/FVC %.
D. Increased TLC.
E. Increased airway resistance when related to lung volume.
Answer: C
94. The arterial hypoxemia of a patient with diffuse interstitial pulmonary fibrosis:
A. Typically worsens on exercise.
B. Is chiefly caused by diffusion impairment.
C. Is associated with a large increase in diffusing capacity during exercise.
D. Is usually associated with carbon dioxide retention.
E. Is improved during exercise because of the abnormally large increase in cardiac output.
Answer: A
95. In a patient with diffuse interstitial fibrosis of the lung, the maximal expiratory flow rate at a given lung volume may be higher than in a normal SBject because:
A. Expiratory muscles have a large mechanical advantage.
B. Airways have a small diameter.
C. Dynamic compression of the airways is more likely than in a normal subject.
D. Radial traction on the airways is increased.
E. Airway resistance is increased.
Answer: D
96. The diffusing capacity for carbon monoxide in a patient with diffuse interstitial lung disease:
A. Is typically substantially increased.
B. Shows an abnormally large increase during exercise.
C. Is unaffected by thickening of the blood-gas barrier.
D. Is reduced in part because of obliteration of pulmonary capillaries.
E. Falls only late in the disease.
Answer: D
97. Features of pneumothorax include:
A. It reduces the volume of the chest wall on the affected side.
B. It causes an increased blood flow in the affected lung.
C. When present in the tension form it is a medical emergency.
D. Spontaneous pneumothorax is mainly seen in older women.
E. The FVC is increased
Answer: C
98. Increased movement of fluid from the lumen of pulmonary capillaries into the interstitium can be caused by:
A. Increased permeability of the alveolar epithelial cells.
B. Reduced capillary hydrostatic pressure.
C. Reduced colloid osmotic pressure of the blood.
D. Increased hydrostatic pressure in the interstitial space.
E. Reduced colloid osmotic pressure of the interstitial fluid.
Answer: C
99. Concerning the blood-gas barrier in the normal lung:
A.Fluid can drain through the interstitium of the thick side of the blood-gas barrier.
B. The alveolar epithelium has a high permeability for water.
C. The strength of the barrier on the thin side is mainly attributable to the endothelial cells.
D. No protein normally crosses the capillary endothelium.
E. Water is actively transported into the alveolar spaces by alveolar epithelial cells.
Answer: A
100. The vast majority of meningitis cases are caused by suppurative bacteria and the organsim relates to the sex of the patient.
A. True
B. False
Answer: B
![MCQs [2024]](https://engineeringinterviewquestions.com/wp-content/uploads/2021/02/Interview-Questions-2.png)